Podcast: Play in new window | Download
Subscribe: Apple Podcasts | Spotify | Android | Pandora | iHeartRadio | TuneIn | RSS

We explore the cutting edge practice of point-of-care ultrasound of the brain, including optic nerve sheath measurement, transcranial doppler, assessing midline shift, and more, with Aarti Sarwal, neurologist and neurointensivist, director of the neurocritical care unit at Wake Forest, and director of their neurovascular lab and ultrasound courses.
References
Anatomy
Literature and guidelines
Pupil reactivity assessment
Doppler patterns
Midline shift
Takeaway lessons
- POCUS can potentially be used to identify elevated ICP by optic nerve sheath ultrasound or pupillary assessment (in patients with difficult-to-assess pupils due to edema or other factors). Midline shift can be seen and quantified via the temporal window, and hemorrhagic masses can potentially be visualized. Finally, spectral doppler of the cranial vessels can show changes in intracranial compliance, similar to that seen in formal TCDs during vasospasm.
- Learning curve for these studies is probably around 50-100 studies until competence, but may be creeping closer to 30–50 and eventually lower due to improving education, and increasing awareness and skills with the general concepts being applied.
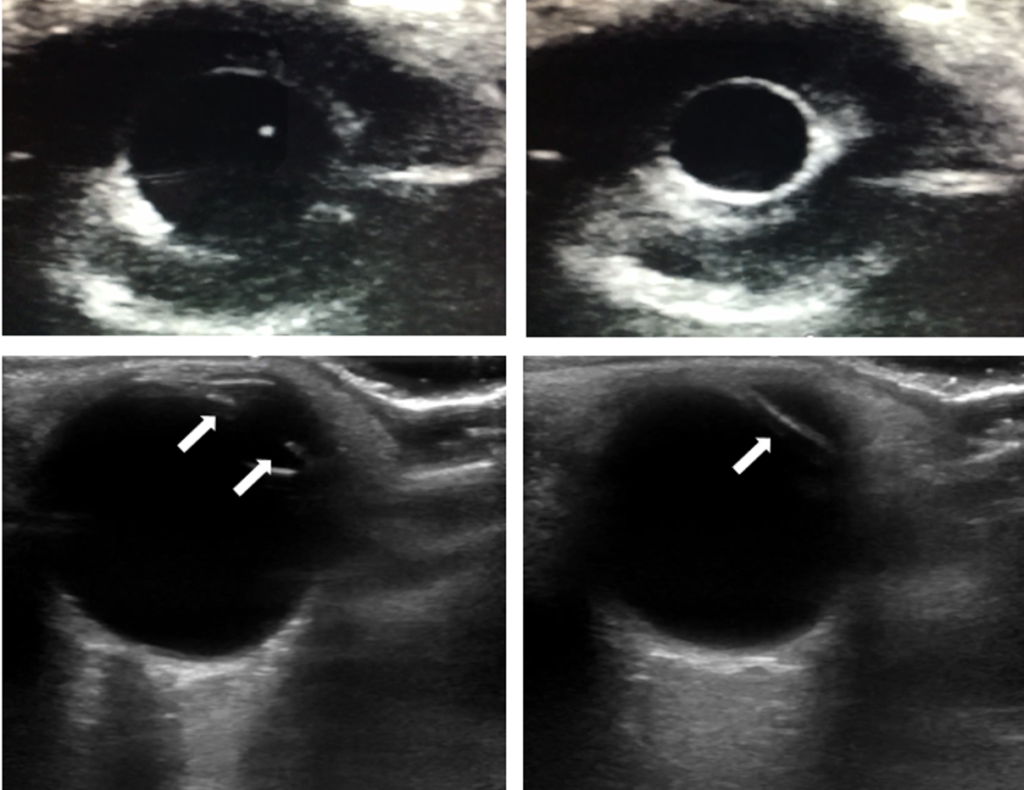
- The linear probe can be used over a closed eyelid to visualize the iris, allowing assessment of pupil response when light in shined in the opposite eye; this can be useful when the lid cannot be opened, such as from edema or trauma. M-mode can even be used for quantitative pupillometry.
- An increased diameter of the optic nerve sheath measured 3 mm from the globe (using the linear probe in a transverse, ear-to-ear axis) correlates with increased intracranial pressure, as the sheath is a continuation of the cranial space and tends to swell with higher ICP. Papilledema can also be seen here as bulging of the optic disc. Use the orbital or ocular preset, which reduces power (mechanical and thermal indexes) delivered to the eye.
- A cutoff reflecting elevated ICP is usually somewhere in the 5-7 mm range. However, normal values vary a lot, and very acute ICP crisis can choke off the continuity and cause normal diameters, so simple measurement can imperfect (analogy: IVC measurement). Trending can be more useful if you can establish a baseline, and papilledema is somewhat more specific. In pediatrics, adjusting for head circumference can help.
- Slower increases in ICP tend to be associated with larger optic nerve sheath diameters, whereas rapid increases may actually be associated with normal sheath diameter, due to edema at the basal cistern level choking off communication with the cranial vault.
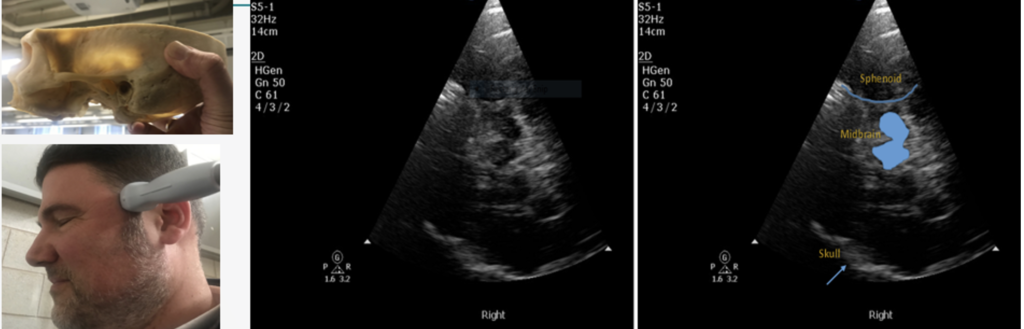
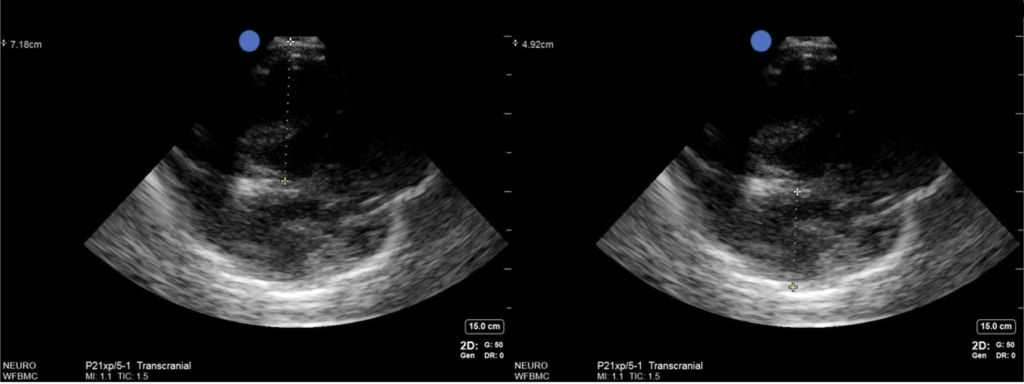
- Midline structures like the pineal gland, third ventricle, or septum pellucidum can be seen from the temporal ultrasound window; 85-95% of the population will have adequate windows here, at least on one side, with some decrease in old age. Males tend to have worse windows, windows worsen over time, and there is some ethnic variation.
- Research is early, but distance of the midline structures from the probe can be compared with their distance from the opposite skull (i.e. in the deep field). Differences between the two can help diagnose and quantify midline shift. Caveats: it’s difficult to establish exactly the same angle when insonating opposing sides, and identical angles can be impossible due to limitations in the windows, so don’t compare that way. The region of edema may mean different structures are shifted while others are normal, or even that there is no shift (e.g. herniation is not lateral); ideally, pick a midline structure that makes sense for where their pathology is found. This is probably more useful for serial comparisons than absolute values, since your angle that penetrates the small temporal window will usually not be perfectly flat, but will be reproducible.
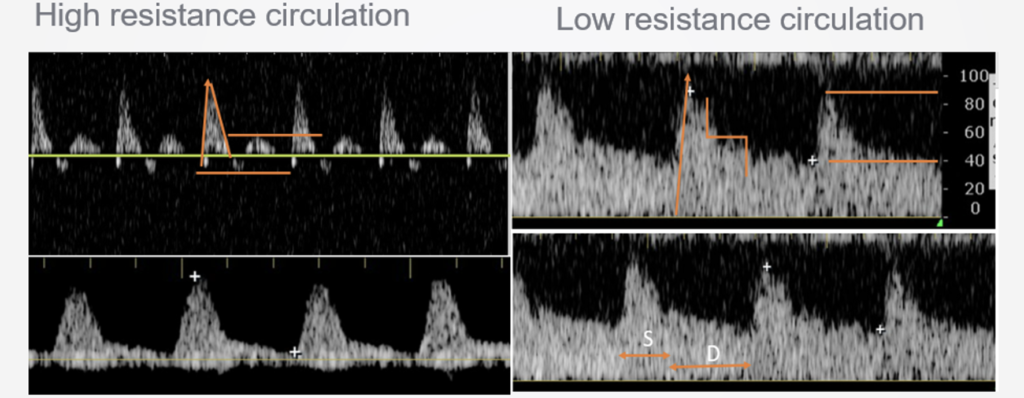
- Global edema may not be seen in midline shift, but may be seen in the TCD waveforms. Spectral doppler of vessels like the MCAs should show low resistance waveforms in a normal brain (low systolic peaks, a long runoff and high diastolic), while in a tighter brain with higher ICP, resistance gets worse, with a higher systolic, quicker drop, and lower diastolic pressure, all the way up until diastolic pressures become less than zero and flow is oscillating (e.g. back-and-forth during the cardiac cycle, which reflects no overall flow and is consistent with brain death). TCD measurements can be directly extrapolated to ICP using a number of published formulas.
- Research is early, but transtemporal B-mode seems to have good sensitivity (>95%) for detecting parenchymal hemorrhage in the brain, as long as it is large and fresh; new blood shows up as a hyperechoic lesion with shadowing.
