Podcast: Play in new window | Download
Subscribe: Apple Podcasts | Spotify | Android | Pandora | iHeartRadio | TuneIn | RSS
Educational critical care scenarios presented in a podcast format.
Podcast: Play in new window | Download
Subscribe: Apple Podcasts | Spotify | Android | Pandora | iHeartRadio | TuneIn | RSS
Podcast: Play in new window | Download
Subscribe: Apple Podcasts | Spotify | Android | Pandora | iHeartRadio | TuneIn | RSS
Podcast: Play in new window | Download
Subscribe: Apple Podcasts | Spotify | Android | Pandora | iHeartRadio | TuneIn | RSS
Podcast: Play in new window | Download
Subscribe: Apple Podcasts | Spotify | Android | Pandora | iHeartRadio | TuneIn | RSS
Visit the Intensive Care Academy
Podcast: Play in new window | Download
Subscribe: Apple Podcasts | Spotify | Android | Pandora | iHeartRadio | TuneIn | RSS
We share our grand new project, the Intensive Care Academy, an online, video-based, subscriber-only educational platform. Check it out at icu101.com!
Podcast: Play in new window | Download
Subscribe: Apple Podcasts | Spotify | Android | Pandora | iHeartRadio | TuneIn | RSS
The COVID-19 pandemic will hopefully wind down this year. What happens next with these patients? A powerful discussion with Eve Leckie (@browofjustice), RN, CCRN, formerly of the CVCC at Dartmouth-Hitchcock and now disabled after contracting COVID. Learn about their acute course of illness, the challenges of navigating the healthcare system with this new disease, and their persistent, poorly-understood symptoms.
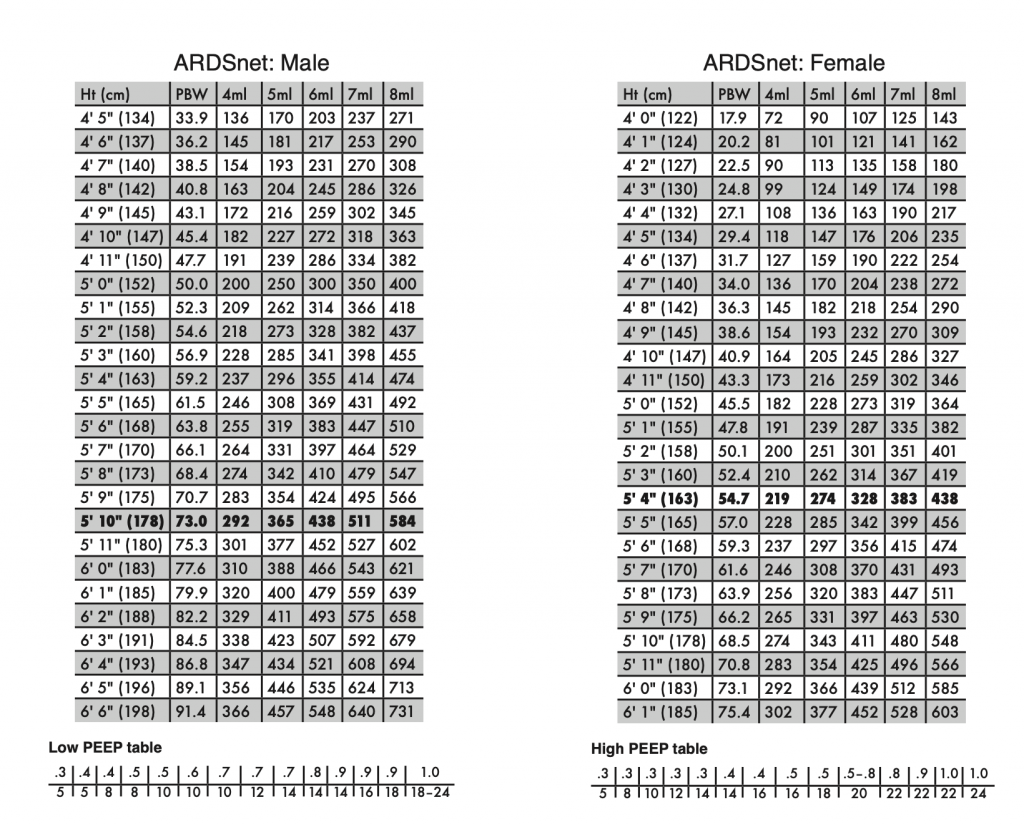
A 5-minute episode describing three hyper-simple, generally safe recipes for the initial strategy of mechanical ventilation after intubating a COVID-19 patient.
Caveat: this is intended for trained clinicians, such as emergency medicine providers, who already have a general understanding of safe and sound life support practices. It glosses over a great deal and is not meant as a primer for trainees.
Podcast: Play in new window | Download
Subscribe: Apple Podcasts | Spotify | Android | Pandora | iHeartRadio | TuneIn | RSS
A fast-tracked update: what we know about the active pandemic of the novel coronavirus (SARS-CoV-2) and its resulting respiratory syndrome, COVID-19.
Podcast: Play in new window | Download
Subscribe: Apple Podcasts | Spotify | Android | Pandora | iHeartRadio | TuneIn | RSS
Getting to know the podcast, your hosts, and why we’re all here in this digital classroom.