Podcast: Play in new window | Download
Subscribe: Apple Podcasts | Spotify | Android | Pandora | iHeartRadio | TuneIn | RSS
The book
Buy the new textbook (Bryan edited, Brandon authored a chapter) here or on Amazon:
Concepts in Surgical Critical Care, First Edition
ed. Bryan Boling, DNP, ACNP; Kevin Hatton, MD, FCCM; Tonja Hartjes, DNP, ACNP-BC, CCRN, FAANP
The podcast
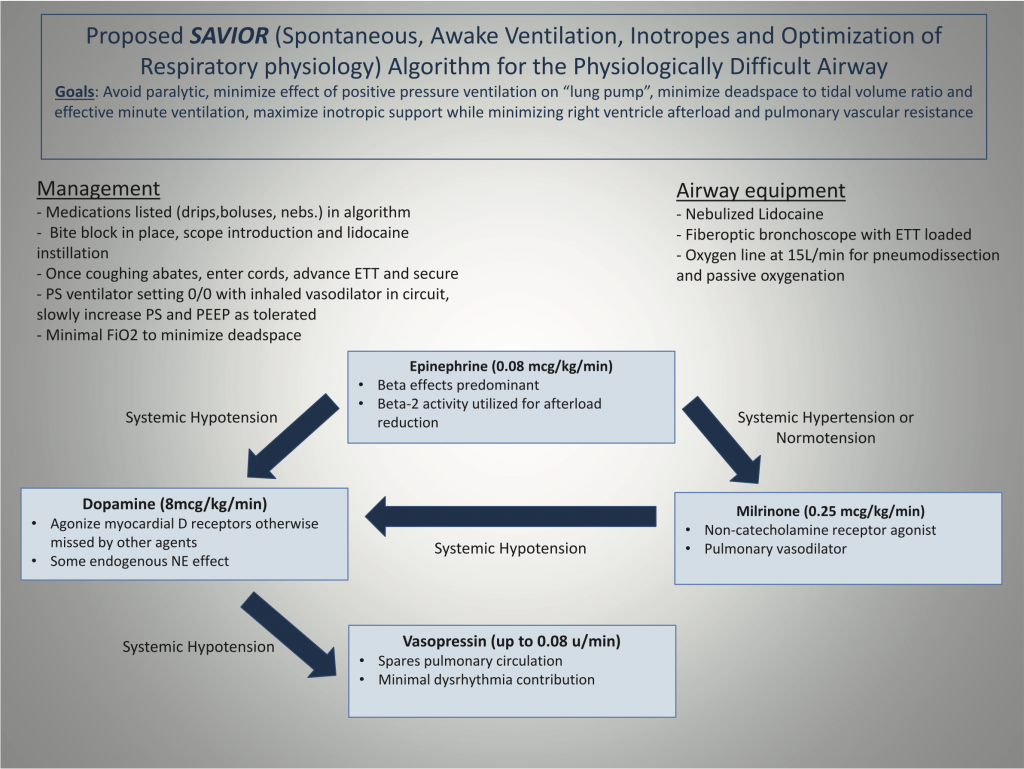
The second piece of our in-depth look at the management of right heart failure, with a focus on preserving peri-intubation hemodynamics using the SAVIOR protocol—featuring its co-creator, anesthesiologist and intensivist from the University of Kentucky, Habib Srour. Check out part 1 here.
Takeaway lessons
- You don’t want to intubate patients with right heart failure, but if you do, you don’t want to do it in a hurry; a well-prepared approach will be far safer. That means doing it at the right time, not sooner and not later, and making what preparations you can before they’re needed.
- Using awake intubation to gently transitioning from spontaneous breathing to mechanical ventilation via up-titration of pressure support (starting at zero) offers a gradual, reversible approach.
- Sedation is often not needed for intubation. The KPET rule gives guidance if desired, but really only applies in isolation; combining drugs creates synergy in their effect and less is often needed.
- 1 mg/kg ketamine
- 2 mg/kg propofol
- .3 mg/kg etomidate
- 4 mg/kg thiopental
Resources
References
- Srour H, Shy J, Klinger Z, Kolodziej A, Hatton KW. Airway Management and Positive Pressure Ventilation in Severe Right Ventricular Failure: SAVIOR Algorithm. J Cardiothorac Vasc Anesth. 2020;34(1):305‐306. doi:10.1053/j.jvca.2019.05.046

Hi guys,
I’m an IM resident interested in critical care, and I love your podcast. Its very informative, and I love how you go through your thought process in each situation and explain why you make the decisions you do. Keep up the good work!
While listening to the episode all I could think was why don’t we just use negative pressure ventilation in these patients? I guess hospitals probably don’t have iron lung machines anymore. But they can’t be that expensive to develop (relative to other healthcare costs anyway). I did some digging and I found a British company that created a modern version of the iron lung in response to the shortage of ventilators during the COVID-19 pandemic. Could technology like this be used to ventilate patients with right heart failure safely?
https://www.exovent.info/
Pouria,
Not a bad question. A few reasons are that it’s harder to care for patients undergoing negative pressure ventilation (the chest is hidden in a cuirass), you can’t really provide PEEP, and it’s not necessarily any more lung protective. (That is, while you’re not introducing high alveolar pressures, you are creating a negative intrapleural pressure, so the transpulmonary gradient may still be high.) Plus there just isn’t much data, as essentially all research on mechanical ventilation for the past fifty years has used positive pressure. It may be that there are still specific use-cases where negative pressure would make sense, but I think they may be lost in the overall milieu.